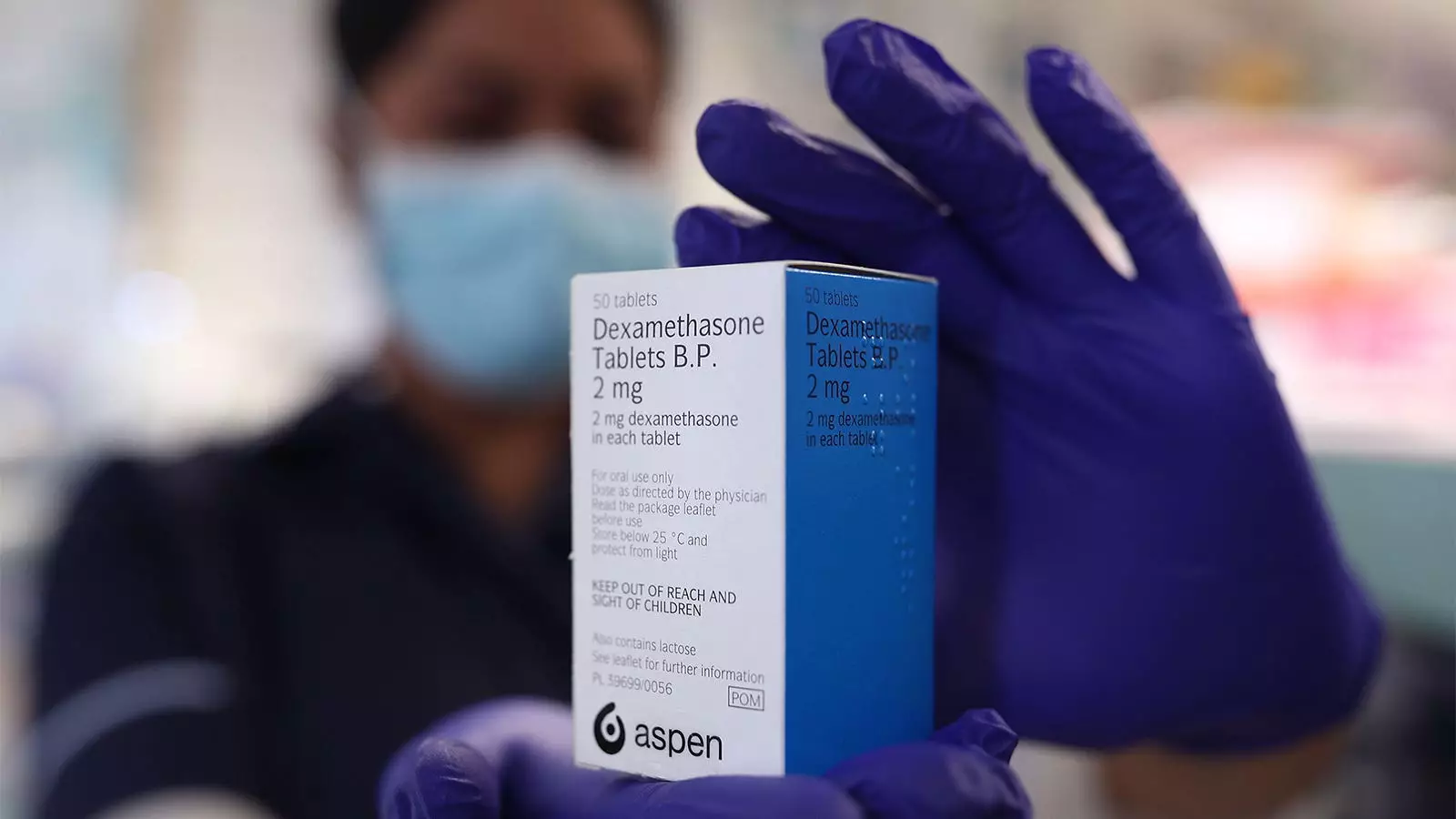
The addition of dexamethasone to the treatment regimen for tuberculous (TB) meningitis in heavily immunosuppressed HIV-positive patients has been a topic of interest and debate. A recent randomized controlled trial conducted in low-resource settings aimed to determine the impact of dexamethasone in improving survival rates and other outcomes among this patient population. This article critically examines the findings of the trial and explores the implications of the study’s limitations.
The Trial and its Findings
The trial included 520 HIV-positive adults from Vietnam and Indonesia who received a year of chemotherapy for TB meningitis. Among the participants, 44.1% who also received dexamethasone died during the 12 months of follow-up, compared to 49% of those who received a placebo. However, the difference in survival rates was not statistically significant (HR 0.85, 95% CI 0.66-1.10, P=0.22). Furthermore, none of the pre-specified subgroups analyzed showed any significant benefits from dexamethasone.
Traditionally, glucocorticoids, including dexamethasone, have been recommended as adjunctive treatment for all patients with TB meningitis, regardless of their HIV status. However, the trial findings challenge this conventional wisdom. The study suggests that the intracerebral inflammation seen in HIV-associated TB meningitis may differ qualitatively from that in TB meningitis unrelated to HIV. The mechanisms leading to death may also vary between HIV-positive and HIV-negative individuals. These distinctions raise questions about the efficacy of dexamethasone specifically in HIV-positive patients with TB meningitis.
While the trial results have more global and international implications, the study highlights the importance of considering the unique characteristics of the patient population in low-resource settings. The majority of the trial participants were heavily immunosuppressed, making the findings primarily relevant to adults with HIV in developing countries. In regions with better-controlled HIV and higher-quality healthcare, the use of dexamethasone might yield different outcomes.
The lack of conclusive evidence regarding the benefit of dexamethasone in HIV-positive patients with TB meningitis necessitates exploring alternative therapeutic approaches. The editorial accompanying the trial suggests a more targeted approach to immune modulation with therapeutics, such as tumor necrosis factor α blockers, and investigation of other therapeutic targets in this population. This would involve tailoring the treatment to the specific clinical phenotypes and varying host responses to TB meningitis.
The trial does not definitively establish the superiority or inferiority of dexamethasone in the treatment of TB meningitis in HIV-positive patients. Larger trials are needed to confirm or refute the presence of a smaller true effect that might have been missed in this study. Additionally, it is important to consider the limitations of the trial, such as the use of open-label glucocorticoids by a significant proportion of participants and the potential for outcome differences to be obscured.
Given the severity and high mortality of TB meningitis, the use of glucocorticoids, including dexamethasone, may still be justifiable despite the lack of significant benefits observed in this trial. It is crucial to individualize treatment decisions based on factors such as the patient’s level of immunosuppression and the control of their HIV infection. Physicians might consider cautiously administering steroids in the hope of a small benefit, with the reassurance that short-term usage would not harm the patient.
Addressing the Root of the Problem
Expanding programs like the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) could contribute to the prevention of TB meningitis by increasing the number of individuals with HIV who are on therapy. Managing HIV effectively can significantly reduce the risk of developing TB meningitis. Furthermore, it is crucial to explore other comprehensive strategies beyond the use of glucocorticoids to address both the prevention and treatment aspects of this challenging disease.
The trial evaluating the use of dexamethasone in the treatment of TB meningitis among heavily immunosuppressed HIV-positive patients provides valuable insights into the complexities of managing this disease in low-resource settings. While the trial did not demonstrate significant benefits from dexamethasone, it prompts further investigation into alternative treatment approaches and highlights the need for tailored interventions based on individual patient characteristics. The findings emphasize the importance of holistic strategies to address the underlying causes and risk factors of TB meningitis in HIV-positive populations.

Leave a Reply