The PREDICT prognostication tool has been evaluated for its ability to estimate overall survival (OS) in a large independent U.S. dataset of breast cancer patients. Researchers from Case Western Reserve University School of Medicine in Cleveland conducted the study using data from the National Cancer Database (NCDB). Their findings, published in the Journal of the National Comprehensive Cancer Network, indicate that PREDICT provided decent accuracy in estimating survival rates when compared to observed rates.
The study analyzed data from over 700,000 breast cancer patients in the NCDB and compared the estimated 5-year and 10-year OS rates generated by PREDICT with the actual observed rates. The median and mean 5-year OS rates estimated by the tool ranged from 83.3% to 84.4%, while the observed rate was 89.7%. Similarly, the estimated 10-year OS rates ranged from 69.4% to 73.8%, whereas the observed rate was 78.7%.
To measure PREDICT’s performance, the researchers used the area under the curve (AUC) of time-dependent receiver operating characteristic curves. The AUC values for survival at 5 and 10 years were found to be 0.78 and 0.76, respectively. These values indicate that PREDICT’s discrimination in estimating survival rates was fairly accurate.
Although the researchers concluded that PREDICT is a useful tool for medical oncologists in estimating clinical risk and the impact of adjuvant therapies on OS, an accompanying commentary highlights that no prediction model can be entirely perfect. The commentary, written by Paul D.P. Pharoah of Cedars-Sinai Medical Center in Los Angeles, acknowledges PREDICT’s calibration and discrimination within acceptable limits but emphasizes the need for caution in relying solely on its predictions.
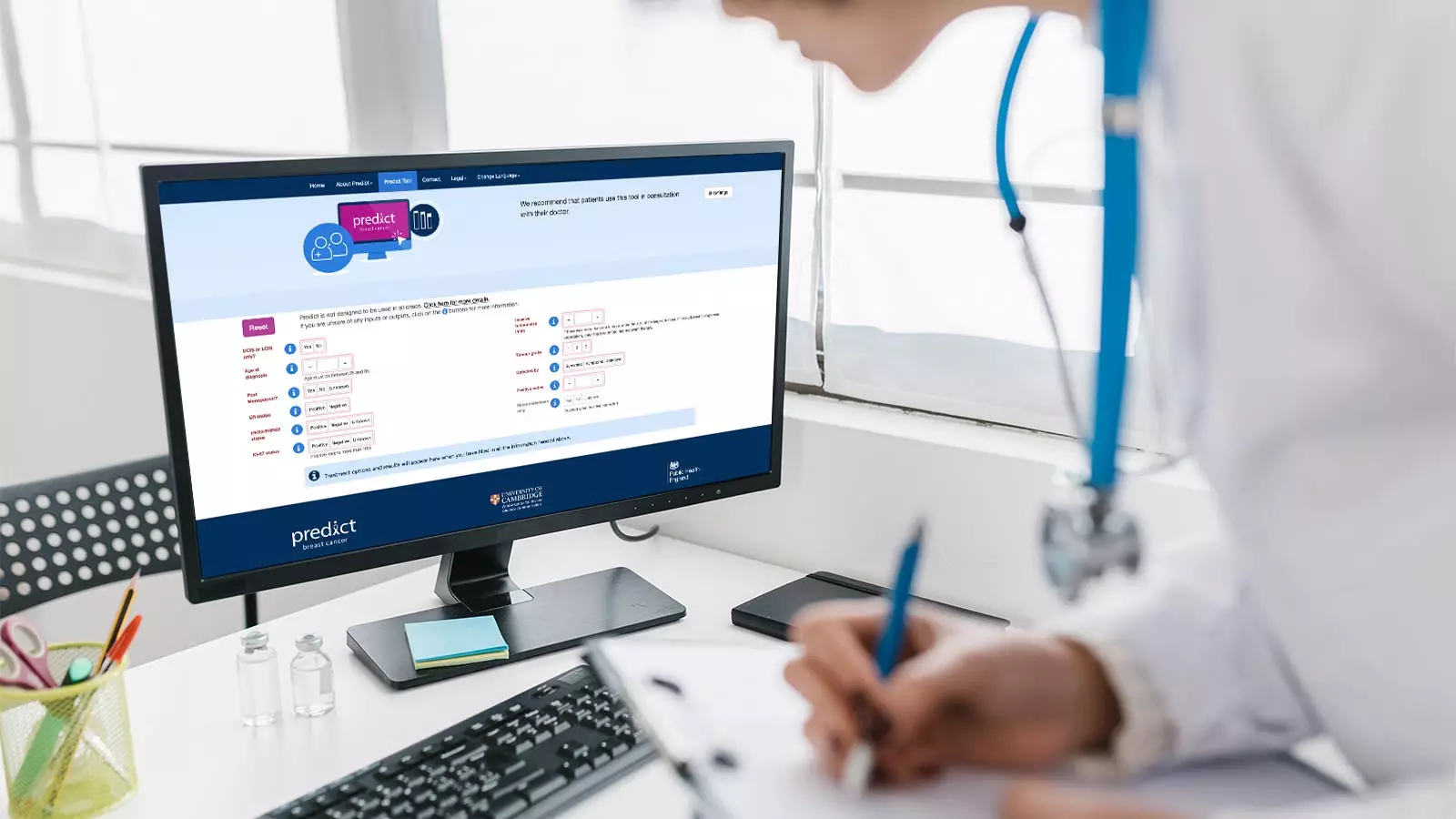
PREDICT is a widely used web-based tool that estimates the risk of dying from breast cancer and the potential benefit of adjuvant therapies on OS. While the tool has previously been validated in other countries and populations, this study represents the first validation in a large U.S.-based dataset of breast cancer patients.
The researchers examined data from 708,652 breast cancer patients in the NCDB diagnosed with primary unilateral invasive disease between 2004 and 2012. To be included in the study, patients were required to have at least 5 years of follow-up. The majority of the patients were white (85.4%), non-Hispanic (88.4%), and had private health insurance (59.2%). Most patients had low comorbidity scores, were from metropolitan areas, and were diagnosed with estrogen receptor-positive breast cancer.
The study found that PREDICT performed best in certain patient subgroups. Black patients, non-Hispanic patients, those with stage I breast cancer, those with estrogen receptor-positive disease, those with HER2-negative disease, and patients receiving adjuvant endocrine therapy only had more accurate survival predictions. On the other hand, PREDICT’s performance was less accurate for patients with high Charlson-Deyo comorbidity scores, as it tended to overestimate survival in this group.
The researchers acknowledged several limitations of their study. One limitation was that the NCDB did not provide detailed treatment data, such as the type or duration of adjuvant chemotherapy or endocrine therapy. Additionally, the study excluded patients who received neoadjuvant therapy, which is the standard of care for certain types of breast cancer. Another important limitation mentioned in the commentary is that PREDICT’s performance is based on all-cause mortality rather than breast cancer-specific mortality. This aspect is crucial since the tool aims to estimate the benefit of systemic therapies on breast cancer-specific mortality.
The PREDICT prognostication tool demonstrated decent accuracy in estimating overall survival rates for breast cancer patients in a large U.S.-based dataset. The tool’s performance was measured using AUC values, which indicated reasonable discrimination in predicting survival rates at 5 and 10 years. While the validation study supports PREDICT’s usefulness as a decision aid for patients and oncologists, it is crucial to consider the limitations of any prediction model. Continued research and validation are necessary to refine and improve the accuracy of prognostication tools like PREDICT for optimal clinical decision-making in breast cancer treatment.

Leave a Reply